In Chasimba, Kilifi South, malaria is not just a disease, it is a constant visitor. For Mariam Katana, caring for her 15‑year‑old granddaughter Joyce, who has battled malaria for two days, the illness feels like a permanent member of the household. Sitting outside her modest home, Mariam explains how malaria has become a routine part of life.
“My son had it last week and went to the hospital. He was treated and given medicine, and after a few days he felt better. Luckily, he had some medicine left, so Joyce is using that while we monitor her. The hospital is far, and that is why we always keep spare drugs at home. It feels like we are always prepared for the next person who falls sick. Malaria has become something we live with, like it is part of the family,” she narrates sadly.
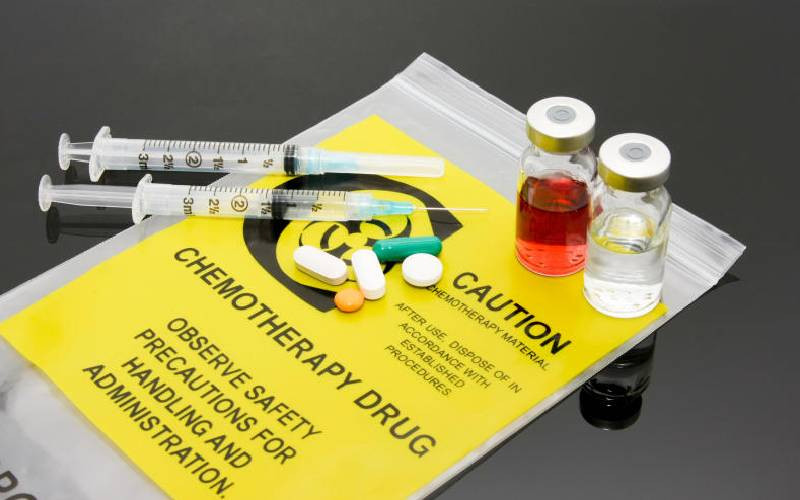
Her words reflect a reality that many households in Kilifi South know too well. Leftover drugs have become common and, while they symbolize resilience in the face of limited access to healthcare, they also carry risks. Yet for families like Mariam’s, the choice often feels like survival rather than negligence.
Rukia Ngonyo, a young malaria awareness advocate in Kilifi and the wider coastal region, has dedicated her voice to demystify narratives around the disease.
“I grew up seeing how often children missed school because of malaria, how families struggled with hospital costs and how the disease kept coming back. I wanted to use my voice to make people understand that malaria is preventable and that communities can protect themselves if they are empowered with the right knowledge.”
Rukia’s recalls standing in front of classrooms, speaking to students about mosquito nets, and later seeing those same children go home and remind their parents to use them.
“I believe communities are empowered when they understand the risks and prevention methods. When young people hear the message, they carry it home. I have seen children sing malaria rhymes and convince their parents to cover water containers or sleep under treated mosquito nets. That is the kind of change we need, change that starts small but grows into community responsibility.”
From her work, Rukia identifies the main drivers of malaria in Kilifi: stagnant water and poor drainage, limited use of treated mosquito nets, poverty, gaps in awareness, the humid coastal climate that favours mosquitoes and misuse of the prescribed drugs.
“People are not following the doctor’s full directions, but it is not just about medicine. It is about how we live, how we store water, how we protect ourselves at night. Malaria thrives where there is poverty and neglect and that is why awareness is so important.”
Social behaviour change
Despite Kilifi County’s overall decline in malaria prevalence—from 8 per cent to below 5 per cent in the past five years—Kilifi South continues to record significant case numbers, with sharp monthly and annual fluctuations.
Data from 2023 to 2025 shows a bimodal seasonal pattern, with peaks following the rainy seasons in April to June and October to December.
In 2023, high cases were recorded in January, with peaks in May and September. In 2024, the worst year, January saw a spike of 2,434 cases and September reached a record 2,867.
In 2025, the highest January spike yet was recorded at 3,117 cases, followed by another surge in July with 2,392.
Across all three years, January, May, July and September consistently recorded high transmission, while February and April saw lower numbers. This variability highlights the complex and changing epidemiology of malaria in coastal Kenya.
Kilifi’s malaria control strategy has gone beyond medical interventions, embracing social behaviour change to mobilize communities creatively.
Football matches became awareness platforms, with players donning jerseys inscribed ‘Sisi Ndani, Mbu Nje’. Popular bands composed catchy songs with prevention messages, performed at weddings and social gatherings.
Pageants such as Mr and Miss Malaria Control and soccer events specifically targeted adolescents, who often underestimate their risk.
Kaya elders have played a key role in dispelling myths, including fears that mosquito nets were unsafe.
Trained community health workers visited households to ensure proper net use, treatment compliance and ongoing education. Schoolchildren sang malaria-themed rhymes, carrying prevention messages into their homes. Together, these efforts transformed prevention into a cultural movement, embedding health messages into everyday life.
“Our efforts have borne fruit, but the situation in Kilifi South remains challenging. During my engagement with the community, I discovered that many people do not take malaria prescriptions or doctors’ dosage instructions seriously.
Most patients stop medication once they feel slightly better and the remaining drugs are then used by the next person who falls sick. Another problem is improper storage of water for domestic use, most containers are uncovered, creating breeding spots for mosquitoes inside homes.
Despite efforts like distributing treated nets, the gaps in Kilifi South are still huge. We need more household-level education, greater treatment compliance and more responsibility in how families store water,” shares Kilifi County Malaria Control Coordinator Chimanga Mwamuye.
Speaking on this trend, Kilifi-based medic Elizabeth Gathua highlights the dangers of sharing malaria medicines. “Sharing malaria medicines is a recipe for disaster. Not only does the sick person miss the full dose, but the person sharing also exposes themselves to potential health risks. Our standard treatment, Artemether/Lumefantrine, is a powerful combination: artemether rapidly clears the majority of malaria parasites, while lumefantrine continues to eliminate any remaining parasites more slowly.
When medicines are shared, there is a risk of creating stronger, drug-resistant malaria strains that are harder to treat. These resistant strains can spread through mosquito bites, putting entire communities at risk,” she explains.
She adds: “If you are not tested, taking malaria medication can delay diagnosis and worsen your condition. Everyone responds differently to medication and self-prescription can lead to adverse reactions.
Consult a healthcare provider, they are best equipped to prescribe the right treatment for your specific needs. We must prioritize responsible malaria management and protect ourselves, our communities, and future treatments.”
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.