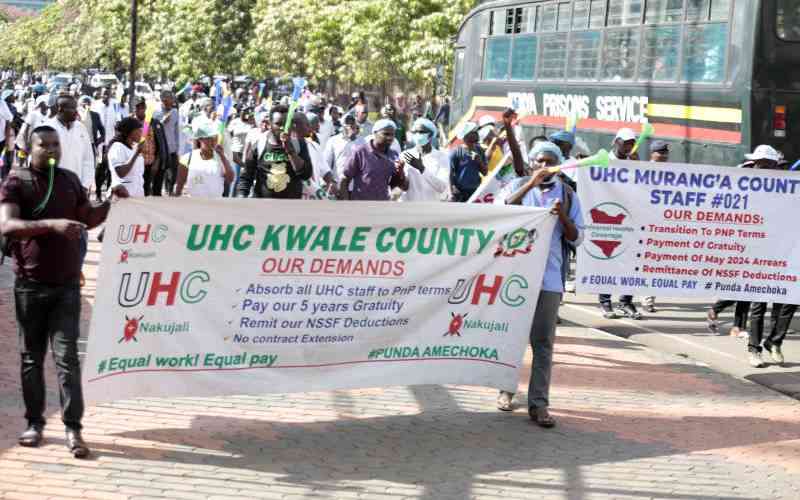
Universal Health Coverage (UHC) staffers from across the country stage a demonstration in Nairobi where they presented their petition to the Parliament on March 11, 2025. [Boniface Okendo, Standard]
×
 The Standard Group Plc is a
multi-media organization with investments in media platforms spanning newspaper
print operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a leading multi-media house in Kenya with a key
influence in matters of national and international interest.
The Standard Group Plc is a
multi-media organization with investments in media platforms spanning newspaper
print operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a leading multi-media house in Kenya with a key
influence in matters of national and international interest.
 The Standard Group Plc is a
multi-media organization with investments in media platforms spanning newspaper
print operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a leading multi-media house in Kenya with a key
influence in matters of national and international interest.
The Standard Group Plc is a
multi-media organization with investments in media platforms spanning newspaper
print operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a leading multi-media house in Kenya with a key
influence in matters of national and international interest.
- Standard Group Plc HQ Office,
- The Standard Group Center,Mombasa Road.
- P.O Box 30080-00100,Nairobi, Kenya.
- Telephone number: 0203222111, 0719012111
- Email: [email protected]
NEWS & CURRENT AFFAIRS
TV STATIONS
RADIO STATIONS
ENTERPRISE