×
The Standard e-Paper
Home To Bold Columnists
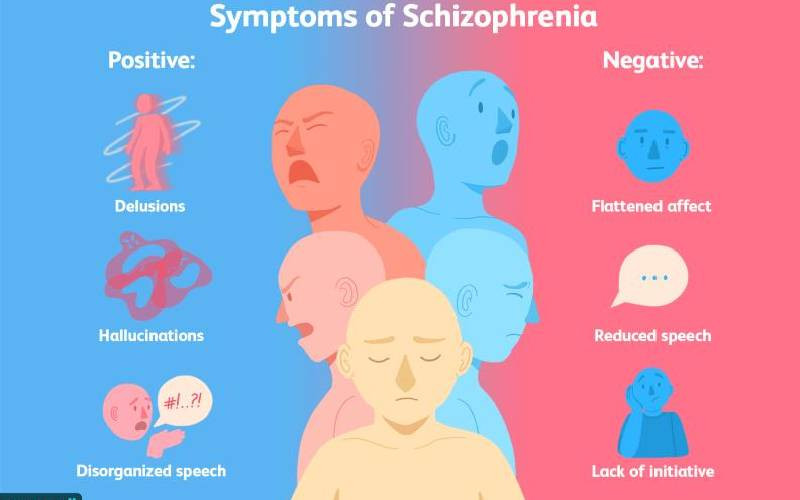
The mental disorders of psychosis and schizophrenia have always been discussed interchangeably even in the medical circles, but there exists a clear delimitation between the two.