Kenya risks losing progress made in eliminating three killer diseases; Malaria, HIV and tuberculosis, due to inadequate domestic funding.
This follows suspension of activities by the United States Agency for International Development (USAID), the Centers for Disease Control and Prevention (CDC), and the President’s Emergency Plan for AIDS Relief (PEPFAR).
The abrupt move has caught Kenya off-guard, with no clear structures in place to transition from foreign aid to sustainable domestic funding. In 2020, Kenya initiated efforts to transition from donor dependency to domestic health financing.
A key component of this strategy was the social public health insurance scheme under the now-defunct National Hospital Insurance Fund (NHIF), a role taken over by the Social Health Authority (SHA).
However, implementation of these financing mechanisms remains incomplete with lack of concrete solutions to address the funding gap.
When contacted by The Standard for comment on the government’s preparedness to handle dwindling donor support, Director General of Health Dr Patrick Amoth was reluctant to elaborate.
He said the matter would be addressed in a press briefing scheduled for today (Wednesday).
- Polio vaccine safe, health ministry assures Kenyans
- Public health facilities to be prioritised in NHIF pending bills payment
- Five new M-pox cases confirmed, including two children
- Social Health Authority disburses Sh1.36 billion since rollout
Keep Reading
In an interview with a local radio station, Senior Deputy Director at the Ministry of Health, Sultani Matendechero, emphasized the need for Kenya to explore domestic philanthropy as an alternative to external donor funding.
“Instead of relying solely on external philanthropy, we also have philanthropists here in Kenya who can plug into the public health space,” said Dr Matendechero. “It is something we are already working on. While we are facing some challenges, as you know, we believe that with time, we will stabilise and increase the injection of domestic resources into public health.”
But Matendechero did not specify who these local philanthropists are or when they would be engaged to support the country’s health system.
Faith Ndung’u, Advocacy Manager at the Health NGOs Network (HENNET), expressed concern over the slow progress in transitioning from donor dependency.
She noted that while Kenya has been discussing donor transition plans, including development of the HIV transition strategy and recent launch of the Kenya Operational Plan for Enhanced Country Readiness to Sustain a Resilient HIV Response Beyond 2030 (marked during World AIDS Day 2024), tangible action in terms of government budget allocation remains limited.
“The discussions have been ongoing, but there has been little translation into actual funding allocations for HIV by the government,” said Ndung’u.
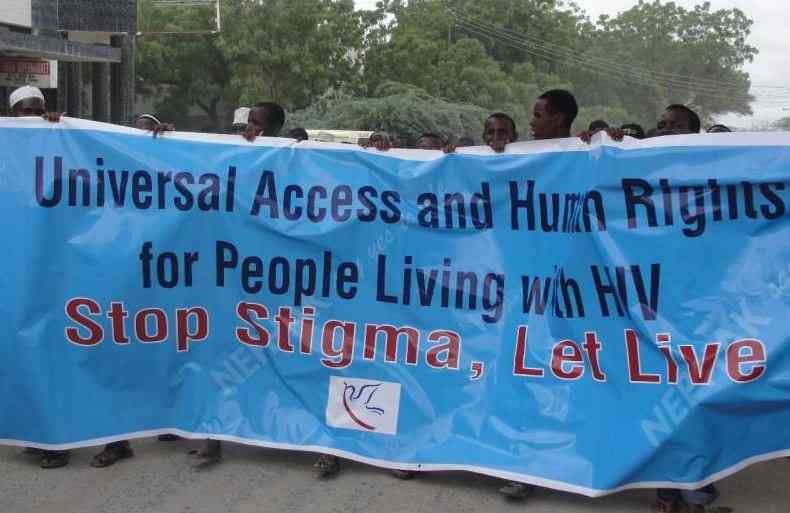
Currently, 1,378,457 Kenyans are living with HIV, with 1,336,681 receiving treatment, reflecting a gradual increase from 1.2 million in 2022.
Treatment of HIV programme is run by PEPFAR, USAID and Global Fund including other partners.
“For us to be resilient, we need to have more funding from the Kenyan government but also have negotiations with donors on staggered transition to avoid gaps in service delivery," added Ndung'u. "In the same regard, we need to also focus on all donor funded programmes, including immunisation".
Regardless of Trump’s executive order, PEPFAR funding for HIV commodities has been shrinking over the years, from Sh17 billion in the past ten years, to the current Sh7.3 billion.
“It is not the first time we are having a funding issue with the donor. The issues have being raised have been here from 2014. Even if PEPFAR comes back, which is likely, Kenya will need to think loud on the response to HIV and TB,” said Director of National Empowerment Network of People Living with HIV/AIDS in Kenya (NEPHAK), Nelson Otwoma.
Otwoma questioned why South Africa and Rwanda procure their drugs, and not Kenya, which is ranked position seven globally in HIV epidemic.
“The Kenya government needs to take up procurement of ARVs for people living with HIV. Even if PEPFAR comes back (which is likely), let them do other work but leave medicines to the government,” observed Otwoma.
In a previous interview, Daniel Mwai, President William Ruto’s health advisor, also a member of donor transition committee, admitted the need for sustainable donor funding.
“Donor fund will is not sustainable, despite it being the vein that supplies blood to our healthcare system. We need to transition,” said Dr Mwai.
With repealing of NHIF in October, at least 18.1 million people have registered with new scheme - SHA.
Kenyan health funding is allocated from the exchequer, donor support, out-of-pocket, insurance, and private investment. Even as donor fund shrinks, the country seems not prepared, for self sustainability.
The central and county governments control about 33.6 percent of health financing scheme.
Data by Ministry of Health reveal that total insurance, both the social and private control around 25 percent of the funding, with NGOs controlling about 16.2 percent, 3.1 percent by the private sector, and about 24 percent being out of pocket, for individuals who do not have insurance.
Before actualisation of SHA, insurance penetration in the country was only 20 percent, with 80 percent of the Kenyan population being without an insurance cover.
But Janefer Kinyanjui, a health economist observes that the new financing model of insurance-SHA has a component of looking into non-communicable diseases and communicable diseases, but its implementation remains unclear.
Allan Maleche, the Executive Director of the Kenya Legal and Ethical Issues Network on HIV and AIDS (KELIN), observes that Kenya lacks a comprehensive domestic funding model to sustain donor-supported programs aimed at eliminating malaria, tuberculosis (TB), and HIV/AIDS.
“We have never been prepared because we have always relied on the consistency of PEPFAR and the Global Fund,” says Maleche.
He explains that the lack of preparedness is evident in the fact that over 60 percent of the support for HIV, TB, and malaria programs comes from the U.S. government and other donors.
Apart from HIV/AIDS response, malaria is among Kenya’s leading cause of deaths.Malaria program also benefit from USA, and other donor support.
According to US Presidential Malaria initiative report by USAID, malaria remains a major public health challenge in Kenya, a disease that accounted for at least 15 percent of outpatient consultations nationally.
The report notes that Kenya has made significant gains in reducing malaria burden, for example from 2010-2020, the prevalence of malaria reduced by 50 percent from 38.1 percent to 18.9 per cent in the high-burden lake-endemic area, with while nationally, the malaria burden decreased 49 per cent to 5.8 per cent.
At least 320, 000 malaria treatment doses procured by USAID for distribution to health facilities, 5 million rapid diagnostic tests delivered for distribution to health facilities and additional 4.9 million Long Lasting Insecticidal Nets procured for distribution to vulnerable populations in high malaria transmission counties.
Over 1.5 million people protected from malaria through indoor residual spraying.
The suspension of US donor aid comes at a time when the country’s budgetary allocation for health continues to decline."
“It is worrying that we never locate adequate budgets to run our health system because at the back of our minds, we know donors will supply us with childhood vaccines, ARVs mosquito nets to stop malaria deaths. We should think outside the box,” says Kinyanjui.
Kenya’s budgetary allocation for health has been reducing over the years.
In 2024/25 financial budget, some Sh127 billion was allocated to the sector, a decrease of Sh11 billion, from Sh138 billion allocated in the 2023/24 financial year.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.