HIV treatment has delivered life-altering advantages. Antiretroviral therapy has led to reduced mortality and improved life expectancy for people living with HIV. Nearly 41 million people were living with HIV in 2024, with Eastern and Southern Africa accounting for 21.1 million and Western and Central Africa accounting for 5.2 million.
However, there are risks associated with the therapy, including the potential for health conditions affecting the heart, blood vessels, and metabolism, such as high blood pressure and excessive weight gain.
Melani Ratih Mahanani, a medical doctor and epidemiologist, unpacks her research conducted in Malawi that showed some drugs have side effects. She emphasises that weight gain or high blood pressure following HIV treatment does not mean the treatment is failing or dangerous.
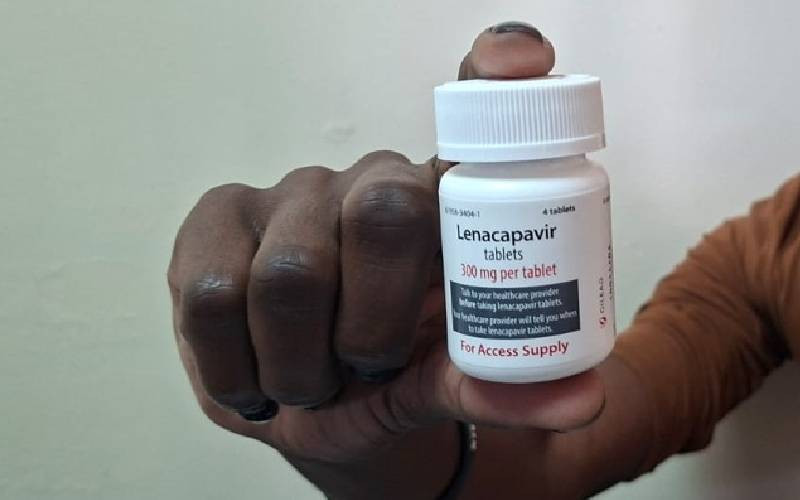
Instead, these patterns indicate that HIV care and chronic disease care need to work together. Modern HIV care depends on antiretroviral therapy as its fundamental component. This therapy consists of a variety of pills that treat HIV by stopping the virus from replicating.
Antiretroviral therapy protects against viral suppression while supporting the immune system and preventing serious illnesses. The suppression of HIV enables people to experience better health and gain more energy to work, study, care for their children, and actively participate in their communities. It also provides dual protection to both patients and their partners.
The therapy decreases the risk of HIV transmission during sex and pregnancy. With it, medical scientists have achieved breakthroughs in HIV treatment, turning HIV/AIDS into a condition that can be managed long-term. Treatment provision in various communities has also decreased stigma, as people on therapy remain visibly healthy and active.
With consistent daily use, antiretroviral therapy allows individuals to live longer. Malawi’s life expectancy was 66.04 years in 2022 and has risen to 66.37 years in 2025. It not only protects individuals’ health but also strengthens families and communities.
The advantages of antiretroviral therapy outweigh potential side effects, which may appear during extended medication use. Nevertheless, it can impact cardiometabolic health, causing high blood pressure or excessive weight gain.
- Over 100 people die by suicide in three months in Nyeri County
- Animal welfare group expands efforts to control rabies with new Watamu branch
- HIV gains at risk as donors cut lifeline support
- Why 'disco matanga' is to blame for high HIV prevalence
Keep Reading
A total of 432 people living with HIV participated in the research, 317 of whom were female. Dolutegravir, recommended in WHO guidelines, has been associated with excess body weight gain, prompting the study to investigate this claim. Data were also retrieved on body weight and systolic blood pressure of 543 people on other drugs—tenofovir and lamivudine—before switching to dolutegravir.
Blood pressure analysis showed that among 432 patients followed, newly diagnosed hypertension was found in 11% after switching to dolutegravir, compared to 5.4% on previous antiretroviral medications. Other drugs, such as efavirenz and tenofovir, were linked to slower but steady increases in heart-related risk over several years. About 24 out of 201 patients (11.9%) experienced a slight worsening of heart-related risk after three years of follow-up.
Weight gain after dolutegravir was minimal. The effects of weight gain and high blood pressure do not affect all patients receiving antiretroviral therapy. Most experience no significant changes in weight or blood pressure, while only a few are affected.
Variations between patients stem from age, diet, physical activity, genetics, and overall health. For example, some patients experienced weight gain or elevated blood pressure during the study, while others did not. Being female, starting treatment with a lower body weight, and having good kidney function appeared to protect against rising blood pressure.
As people living with HIV grow older and remain on lifelong treatment, heart health becomes increasingly important. High blood pressure and excessive weight gain are factors, and some HIV medications can also affect cholesterol levels. These medications may cause inflammation or alter how the body processes fats and sugars.
People with HIV must take antiretroviral therapy daily as prescribed because stopping treatment can allow the virus to rise, weaken the immune system, and increase transmission risk. Alongside adherence, monitoring weight, blood pressure, and overall well-being during routine clinic visits is essential. Regular visits provide an opportunity to check health, ask questions, and catch changes early.
Healthy habits can support overall well-being, including regular physical activity, increased fruit and vegetable intake, and reduced salt consumption. Avoiding smoking and excessive alcohol can also reduce the risk of weight gain and high blood pressure. These habits can be incorporated into daily activities without spending money on equipment or gym memberships.
It is important for patients to speak openly with healthcare providers if they notice rapid weight gain, headaches, dizziness, or other symptoms. These are not signs of treatment failure but indicate that additional support may be needed. Community support groups and peer counsellors can also help people living with HIV stay motivated and share practical ways to remain healthy on therapy.
People living with HIV should stay on treatment, stay informed, and stay connected to care. Healthcare providers and governments share the responsibility to ensure that HIV care addresses both viral suppression and long-term well-being. Routine monitoring of weight, blood pressure, diabetes, and heart health should be integrated into standard HIV care.
Clinics should have the tools to measure blood pressure and provide early treatment for hypertension when needed. Governments can strengthen national guidelines, provide training for health workers, and ensure essential medicines for conditions like hypertension are consistently available. Additionally, they should invest in research and long-term monitoring systems to keep policies responsive to emerging evidence.
At the community level, health facilities can create safe spaces for discussions about weight, diet, and lifestyle without judgment. Public health campaigns can educate people that weight gain after starting antiretroviral therapy is common and manageable, and that monitoring health is a sign of good care. By integrating HIV care with non-communicable disease prevention, healthcare systems can help people living with HIV remain healthy throughout their lifespan.

 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.