Miriam* is a playful six-year-old. As she works on her school assignments, an alarm suddenly rings.
It reminds her of time to take her medicine. She quickly runs to alert her aunt, Joan*.
Miriam is HIV positive, a disease she acquired from her late mother, who died of advanced HIV disease, commonly known as AIDS.
Though Mirriam does not know she has HIV, she understands one thing; “the medicine keeps her alive”.
“Seeing my niece grow every single day warms my heart,” says Joan, who took over Miriam’s care after her sister’s death. When her sister died, Miriam was hanging on to life by a thread.
She was frail and battling Tuberculosis (TB), one of the co-infections that strike when HIV progresses to an advanced stage. “When my sister died, we took Miriam for HIV testing. The results came back positive,” Joan recalls.
“She also had TB, but after six months of treatment, she has recovered.”
Joan pauses, tears of joy streaming down her face. “When I look back, my heart is warm. I never imagined Miriam would survive. She was so weak. I thought she would die, just like her mother.”
- Kenya to vaccinate children against typhoid and measles-rubella
- Missed BCG jabs, leaves newborns at risk of deadly TB
- Killer counterfeits: How fake malaria drugs claim 100,000 lives every year
- Why more newborns are contracting HIV from breastfeeding
Keep Reading
She explains how her sister’s struggle with HIV ended tragically.
Skipped medication
Despite testing positive, she often skipped her medication. The sister moved from Nairobi to stay with her after her health deteriorated.
The virus weakened her body, leaving her vulnerable to TB and meningitis, infections that eventually claimed her life. “My sister suffered in silence,” observes Joan.
She adds, “By the time she was rushed to the hospital, it was too late. Treatment could not save her. She tested HIV positive and had TB”.
At Naivasha Sub-county Hospital, Florence*, a mother of three, shares a similar struggle. She was diagnosed with HIV in 2015 but was not ready to start treatment, thanks to pill fatigue. “I thought I could manage without the drugs,” she admits.
In 2017, her health deteriorated, forcing her back into care.
But in 2019, after regaining strength, she stopped taking her ARVs again. Defaulting caused her to acquire TB, co-infection among HIV patients. AHD caused miscarriage of her four months pregnancy.
But she finally adhered to her treatment, her health improved, her viral load dropped and she conceived again. Today, she is raising a healthy, HIV-negative two-year-old boy. “I look back at my HIV journey and I can only celebrate the milestones,” she says with a smile.
“It has not been easy, but my son gives me the strength to take my ARVs every single day. I live for him and for myself.”
In the same neighbourhood, Zeyn* is still battling meningitis and TB after repeatedly defaulting on his HIV treatment.
“I knew I had HIV, but having gotten a partner, I did not want to disclose, or be seen taking ARVs. I defaulted, only to acquire TB and meningitis,” she says.
These are just a few of the many untold stories of people battling with AHD, with rampart deaths reported in villages across the country.
Aid freeze
In 2024, the country reported 21,007 HIV related deaths, of the deaths, 2,685 are children aged 0-14 years. At least 1,326,336 people are living with HIV.
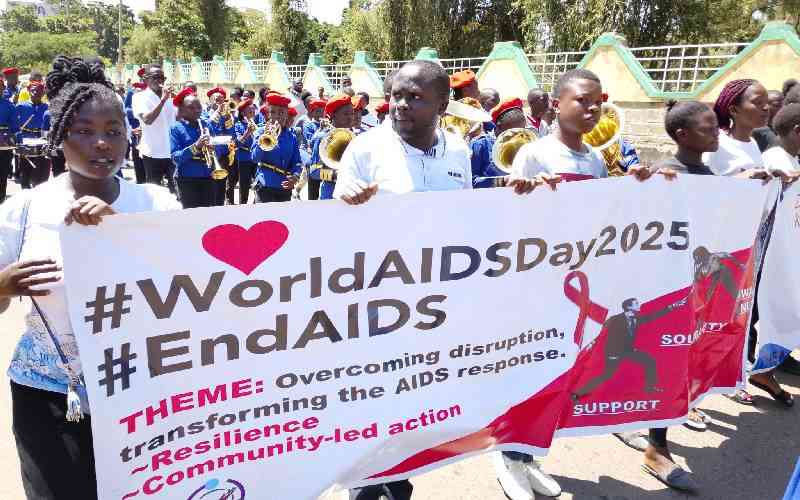
This is a worrying trend, despite years of interventions to end AIDS-related deaths and new HIV infections.
High trends in AIDS deaths saw President Daniel Moi declare HIV a national disaster in 1999, with his predecessor President Kibaki declaring a “total war” against HIV/AIDS in March 2003.
The declarations marked a significant shift towards a more comprehensive and collaborative national response to the epidemic.
Trends in AHD is reported amid freeze on foreign aid, with barely two years shy of Kenya’s target to eliminate new HIV infections and AIDS-related deaths by 2030 and 2027 in paediatrics.
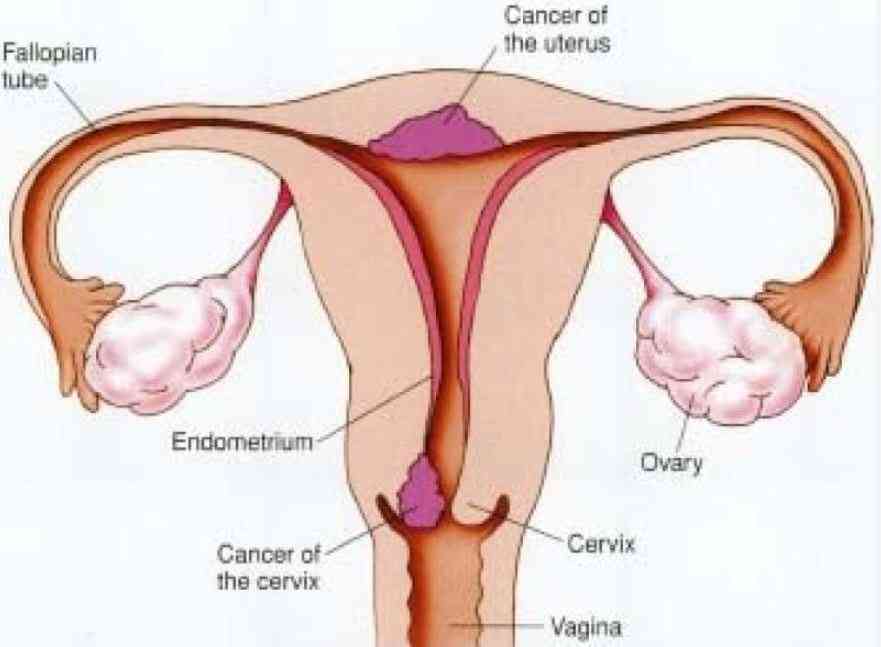
Advanced HIV disease mainly occur as a result of late diagnosis, when immunity is already compromised, failing to enrol for treatment on time and interrupted treatment.
People with AHD are at a great risk of death.
This predisposes them to diseases like TB, cryptococcal meningitis and severe bacterial infections.
Data by National AIDS and STIs Control Programme (NASCOP) shows higher prevalence of AHD in counties with higher HIV burden namely Nairobi, Kiambu, Mombasa and Western.
Head of NASCOP Dr Andrew Mulwa admits that AHD is a national concern even as the country races towards ending new HIV infections and AIDS related deaths. At least 90 per cent of HIV related deaths are attributed to AHD.
“If we have more cases of AHD, it means the programme is failing,” says Mulwa.
He adds, “With AHD means we have more persons living with HIV are not virally suppressed, and, therefore, we have undetectable virus that can spread and are likely to transmit more if they are HIV positive and are not virally suppressed”.
This, he says, cascades infections to all aspects of programming that we have been working on. Kenya begun reporting cases of AHD in 2020.
Disease monitoring
By then, Mulwa notes that more focus had been put in testing and treatment, forgetting the aspect of monitoring of the disease.
“Everyone focused on testing, treatment and viral load suppression. We celebrated earlier, reasons as to why we are seeing re-emergence of deaths,” regrets Mulwa.
Major challenges with AHD is human resource capacity.
“HIV programme has been run as a vertical programme over the years, but with declining donor support, the capacity we have enjoyed over time is not enough to deliver services. One of the challenges to work on is increase capacity of healthcare workers to provide AHD services,” says Mulwa. TB according to data remains a major concern among people living with HIV.
“Unlike other diseases, TB affects the general population and it increases burden of disease in general population. It is, therefore, important to focus on AHD,” says Mulwa. However, Mulwa remains optimistic that with concerted efforts and use of digital platform, Kenya shall end AHD
Among interventions is early screening, treatment and supply of prophylaxis for major opportunistic infections, rapid Anti-retroviral Therapy treatment initiation and intensified adherence support interventions. A visit at Naivasha Sub-County hospital revealed majority of patients reporting with AHD silently die.
The facility serves at least 3,308 HIV positive patients, among them 200 at the facility’s Chronic and Critical Care unit, formally Comprehensive Care Center (CCC).A number of patients seeking care at the center battle with AHD. In September last year, patients presenting with ADH were 200, among them 100 had TB, while 50 had meningitis.
Patricia Kinyanjui, a nursing officer in-charge of the unit, regrets that majority of patients presenting with AHD at the center are at a critical stage. By the time they arrive, they are already battling serious opportunistic infections such TB and meningitis.
“Sadly, we have had cases where patients come in too late. They are admitted and pass away within two days,” says Kinyanjui.
At the unit, patients suspected to have TB are screened for symptoms like persistent fevers and night sweats. The GeneXpert test is also conducted to identify bacteria causing TB.
In addition, CD4 (blood test that determine white blood cell a person has) are performed.
“When a patient’s CD4 count drops below 200, we classify them as having advanced HIV disease,” explains the nurse. “For meningitis cases, a spinal tap is done to analyse fluid from the spinal cord, alongside CD4 testing, to confirm diagnosis.”
At the unit, majority of patients presenting with AHD are men. Men, she says, drop off treatment. “Many men don’t come to the hospital until they are extremely sick,” she says.
Barriers to care and adherence include transport challenges to hospital, pill fatigue and some fear disclosure to partners, while others face food insecurity and social-economic hardships.
Alongside ARV treatment, patients receive other therapies and are linked to support groups. Nakuru, has a network of 3,891 CHPs and peer navigators helping handle AHD.
With support from Clinton Health Access Initiative and USAID Tujenge Jamii, the county has also established four AHD hubs in Naivasha, Bahati, Nakuru PGH and Molo.
Inside they have CD4 machines that run vital tests that guides diagnostic and management of AHD. The County Director of Public Health Elizabeth Kiptoo, says HIV related mortalities stand at between 30 and 70 per cent.
“Hubs have reduced turnaround time for results by nearly 50 per cent, allowing us to diagnose and treat patients earlier, saving lives,” Kiptoo explains.
But major challenge in management of AHD, she admits is commodity stock-outs especially in management of meningitis. Some cases of AHD are also not captured in the county routine reporting tools.
Commodity stock-outs
Apart from AHD, NASCOP has also documented a challenge in eliminating HIV/AIDS in pediatrics. Most children are missing out on diagnosis, treatment and suppression of their viral loads.
Whereas Kenya has surpassed its Global targets of 95:95:95, where at least 98 of the population know their HIV status, 97 are on medication whereas 94 per cent of those on treatment have their viral loads suppressed, pediatrics drag.
As per 2024 data by NASCOP, at least 62,798 children aged 0 to 14 years are living with HIV, among them 4,349 were infected with the virus in 2024. Of the infected, only 75 per cent are on treatment, with 66 per cent viral suppression.
“One thing that makes me not sleep at night is that the president committed to end HIV in children by 2027, which is one and half years away. And that is why we must get solutions on how to get there,” says Mulwa.
As a solution, more focus is being put on Antenatal Clinics (ANC) delivery, post delivery and early childhood HIV.
Apart from pediatrics, infection rates in adolescents and young people, people who inject drugs, men who have sex with men and transgender population and female sex workers is a concern.
Elimination of mother to child transmission remains a major challenge, with data showing at least 9.3 per cent infections in 2024, an increase from 7.3 per cent in 2023.
Nevertheless, Mulwa acknowledges Kenya’s tremendous achievement in eliminating new HIV infections and deaths, since the disease was reported in 1980s.
 The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.
The Standard Group Plc is a multi-media organization with investments in media
platforms spanning newspaper print
operations, television, radio broadcasting, digital and online services. The
Standard Group is recognized as a
leading multi-media house in Kenya with a key influence in matters of national
and international interest.